The Medical Imaging Team
The medical imaging team – physicians, medical physicists, sonographers and medical radiation technologists – works collaboratively to advance a better understanding of the complex practices, policies and protocols behind each image, and to promote the highest standard of appropriate imaging with all Canadians.
The medical imaging team can include:
Interventional Radiologists
 Interventional radiology is the medical specialty devoted to advancing patient care through the innovative integration of clinical and imaging-based diagnosis and minimally invasive therapy.
Interventional radiology is the medical specialty devoted to advancing patient care through the innovative integration of clinical and imaging-based diagnosis and minimally invasive therapy.
Interventional radiologists are doctors who specialize in minimally invasive, targeted treatments performed using imaging for guidance. They use their expertise in reading X-rays, ultrasound, MRI and other diagnostic imaging, to guide tiny instruments, such as catheters, through blood vessels or through the skin to treat diseases without surgery. Interventional radiologists are board-certified and fellowship trained in minimally invasive interventions using imaging guidance.
By combining their expertise in diagnostic radiology with their advanced training in nonsurgical techniques using imaging guidance, interventional radiologists can treat a variety of ailments throughout the body by delivering treatment directly to the source of the problem. Your interventional radiologist will work closely with your primary care or other physician to be sure you receive the best possible care.
Medical Physicists
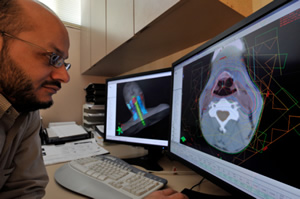 Medical physicists are health care professionals with specialized training in the medical applications of physics. Their work often involves the use of x-rays, ultrasound, magnetic and electric fields, infra-red and ultraviolet light, heat and lasers in diagnosis and therapy. Most medical physicists work in hospital diagnostic imaging departments, cancer treatment facilities, or hospital-based research establishments. Others work in universities, government, and industry. Most medical physicists work in one or more of the following areas:
Medical physicists are health care professionals with specialized training in the medical applications of physics. Their work often involves the use of x-rays, ultrasound, magnetic and electric fields, infra-red and ultraviolet light, heat and lasers in diagnosis and therapy. Most medical physicists work in hospital diagnostic imaging departments, cancer treatment facilities, or hospital-based research establishments. Others work in universities, government, and industry. Most medical physicists work in one or more of the following areas:
Clinical service
The responsibilities of a clinical medical physicist lie predominantly in the areas of radiotherapy and diagnostic imaging. The roles of a medical physicist in radiotherapy include treatment planning and radiotherapy machine design, testing, calibration, and troubleshooting. The roles of a medical physicist in diagnostic imaging include machine purchasing and installation, testing, quality control, and operation.
Radiation safety
Medical physicists have expertise in radiation safety. Canadian regulations recognize medical physicists who are certified by the Canadian College of Physicists in Medicine as Radiation Safety Officers for medical radioisotope facilities.
Medical Radiation Technologists
 Medical Radiation Technologists (MRTs) are an integral part of the healthcare team who perform diagnostic imaging examinations and administer radiation therapy treatments. Upon completion of a CMA-accredited education program that includes both didactic and clinical components at a college or university, graduates are well versed in the application of new imaging and therapeutic technologies. Their course of study includes anatomy, patient positioning, examination techniques, equipment protocols, radiation safety, radiation protection and patient care. Upon completion of their formal education, they are then eligible to write the national certification examination administered by the CAMRT, choosing to specialize in one or more of the four disciplines of medical imaging and radiation science: general radiography, magnetic resonance imaging, nuclear medicine, and radiation therapy. MRTs provide a delicate balance between technical knowledge and adaptive patient skills, generally in a hospital or clinic.
Medical Radiation Technologists (MRTs) are an integral part of the healthcare team who perform diagnostic imaging examinations and administer radiation therapy treatments. Upon completion of a CMA-accredited education program that includes both didactic and clinical components at a college or university, graduates are well versed in the application of new imaging and therapeutic technologies. Their course of study includes anatomy, patient positioning, examination techniques, equipment protocols, radiation safety, radiation protection and patient care. Upon completion of their formal education, they are then eligible to write the national certification examination administered by the CAMRT, choosing to specialize in one or more of the four disciplines of medical imaging and radiation science: general radiography, magnetic resonance imaging, nuclear medicine, and radiation therapy. MRTs provide a delicate balance between technical knowledge and adaptive patient skills, generally in a hospital or clinic.
Nuclear Medicine Physicians
 Nuclear Medicine is an independent specialty accredited by the Royal College. Nuclear medicine is the field of medicine that uses medical isotopes to diagnose, assess and treat patients affected by various diseases both benign and malignant. While cardiovascular diseases and cancers represent a large part of the work of nuclear medicine professionals, most organs in the human body can be investigated by nuclear medicine tests.
Nuclear Medicine is an independent specialty accredited by the Royal College. Nuclear medicine is the field of medicine that uses medical isotopes to diagnose, assess and treat patients affected by various diseases both benign and malignant. While cardiovascular diseases and cancers represent a large part of the work of nuclear medicine professionals, most organs in the human body can be investigated by nuclear medicine tests.
The medical isotopes used in nuclear medicine are also called radiopharmaceuticals. They are injected, swallowed or inhaled by the patient before the study depending on the test to be performed. Medical isotopes mimic the physiology of the human body and use patients’ own molecules to evaluate safely the function of the organs, tissues and cells, diagnose and treat diseases.
Based on the myriad of discoveries that followed the sequencing of the human genome, the nuclear medicine community is currently developing new ways to provide patients a more personalized approach.
Nuclear medicine is practiced by a team of highly trained professionals including nuclear medicine physicians and technologists, physicists, radio-chemists and radio-pharmacists. Some of the physicians practising Nuclear Medicine may also be certified in another speciality such as Internal Medicine, Oncology, Cardiology or Radiology.
The nuclear medicine community aims and traditions are to provide the safest, latest and most appropriate patient care for the citizens of Canada.
Radiologists
Physician specialists in diagnostic imaging
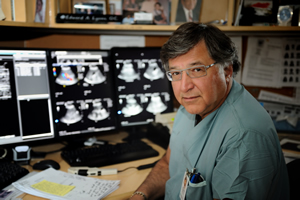 Diagnosing an illness or disease and determining if treatment is working often requires physicians and other healthcare providers to see inside the body and look in ways the human eye cannot. A number of different imaging exams can be used to provide this view, including X-ray, MRI, ultrasound, CT scan, and PET scan. Radiologists are the physicians who specialize in interpreting the results of these imaging exams. Family physicians and other specialists turn to radiologists for consultation on the safest and most effective exam, and what the results mean for the patient and the treatment options.
Diagnosing an illness or disease and determining if treatment is working often requires physicians and other healthcare providers to see inside the body and look in ways the human eye cannot. A number of different imaging exams can be used to provide this view, including X-ray, MRI, ultrasound, CT scan, and PET scan. Radiologists are the physicians who specialize in interpreting the results of these imaging exams. Family physicians and other specialists turn to radiologists for consultation on the safest and most effective exam, and what the results mean for the patient and the treatment options.
In many cases, you will not meet the radiologist who is working on your behalf. You can trust, however, that they have the knowledge and experience to help you and your doctor make informed decisions about your health care.
Sonographers
 Sonographers are an integral part of the healthcare team, playing a critical role by providing key information that facilitates diagnosis and patient management. The quality of an ultrasound study is highly dependent on the skill of the sonographer. In order to perform a thorough ultrasound, the sonographer must adapt their study in response to their sonographic findings.
Sonographers are an integral part of the healthcare team, playing a critical role by providing key information that facilitates diagnosis and patient management. The quality of an ultrasound study is highly dependent on the skill of the sonographer. In order to perform a thorough ultrasound, the sonographer must adapt their study in response to their sonographic findings.
Sonographers bring together an important combination of skills including technical competency, decision making and critical thinking. The sonographer must have an educational background strong in ultrasound physics, anatomy, physiology and pathology. They must analyse data, make judgements, differentiate normal from abnormal, based on real time physiologic information and effectively communicate with patients and other members of the healthcare team. The final diagnostic report relies on information compiled by the sonographer concerning patient history, clinical symptoms and sonographic findings.